Should You Refrigerate Your Medicine? Safe Storage Tips & Facts You Can't Miss

Ever stood in front of your fridge, prescription bottle in hand, uncertain whether your antibiotics or insulin need chilling? This is one of those questions that gets passed around, but half the time, the answer you get leaves you more confused—and occasionally, risking your health. The sneaky thing is, you can't always rely on what your neighbor or even your grandma says. And honestly, storing medicine the wrong way could turn it from healing to harmful.
Understanding How Temperature Affects Medicine
Most medications aren’t as tough as they look. Their chemical compounds can get goofy if the bottle is left somewhere too hot or too cold. But why does temperature matter so much? Well, medicine is basically science in a bottle, and those tiny molecules inside are pretty sensitive.
Here’s some food for thought: the US Food and Drug Administration (FDA) requires all pharma companies to run stability tests at all sorts of temperatures and humidity levels. If the bottle says, "Store at room temperature," the company means it—they’ve tested what happens to the medicine when it sits at 68°F to 77°F (that’s 20° to 25°C, aka what most homes aim for). Suddenly, leaving your allergy meds in a hot car all day doesn’t seem like a great plan, does it? For certain drugs—like insulin, liquid antibiotics, some eye and ear drops—wrong temps can make them less effective or even dangerous.
Think about nitroglycerin tablets, used for heart problems. Set them somewhere steamy like your bathroom, and poof—by the time you need them, they might not work. Penicillin suspensions for kids? If kept out overnight instead of in the fridge, they can lose their punch fast. Another classic: insulin. If you freeze it, it breaks down. Leave it out too long at room temp, it loses efficiency. And don’t get me started on vaccines or certain biologics (like some arthritis injections). These must be kept cold, and even an hour outside the fridge can mean they’re useless.
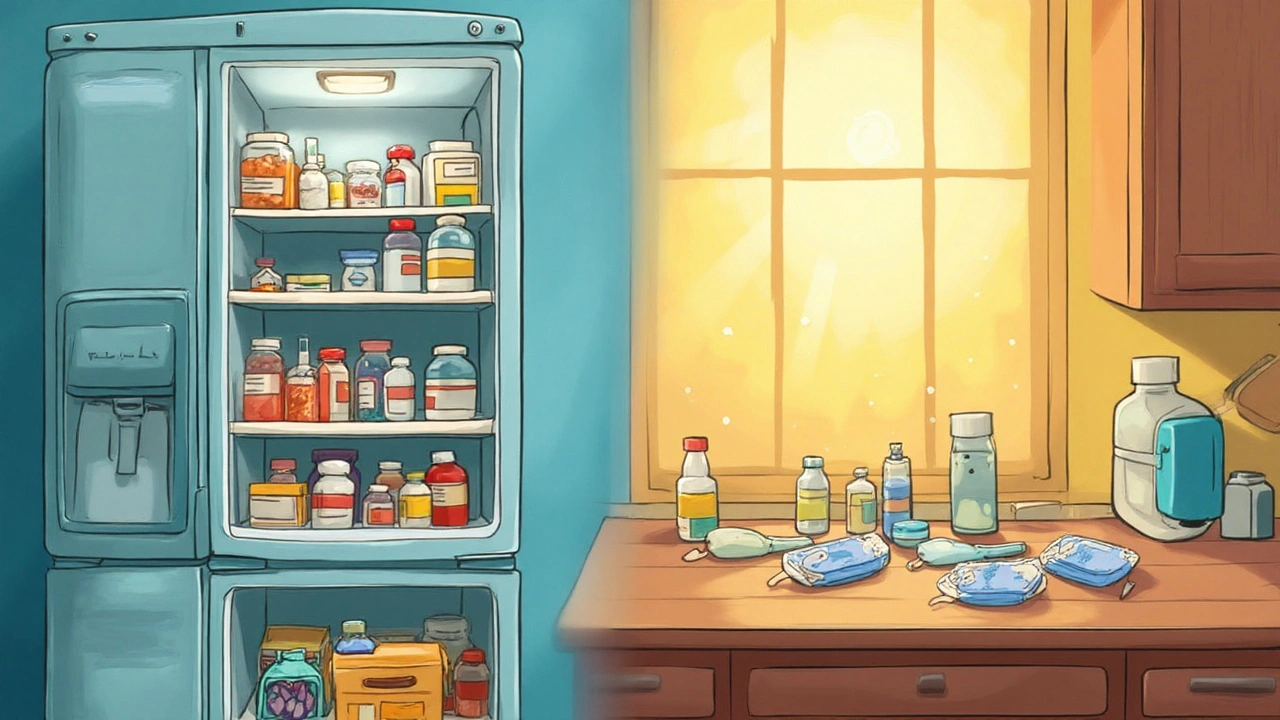
Which Medicines You Should Refrigerate—and Which Ones You Shouldn’t
Here’s a rule: Don’t guess. Always check the prescription label or the leaflet that came with your medicine. Your pharmacist is also your secret weapon; they're usually happy to give you the lowdown without the medical jargon.
Let's break it down with a little cheat sheet:
- Refrigerate these: Most insulins (before they're opened), certain liquid antibiotics (like amoxicillin suspension), many hormone injectables (like growth hormone), some eye and ear drops, some biologics (think Humira, Enbrel), and most vaccines.
- Keep at room temperature: Most pills, capsules, inhalers, and creams—you can store them in a dry, cool place, but definitely not in the bathroom. Humidity and heat are not kind to them.
- Don’t freeze: Insulin, most liquid medicines, and eye or ear drops. Freezing changes their chemistry, sometimes making them dangerous.
Weird fact: There’s a difference between storing your insulin "in use" at room temperature (up to 28 days is safe for certain brands) and new vials/pens that aren’t open yet (those need the fridge). Got eye drops? Most are fine at room temp, but a few require chilling to stay stable.
| Medicine Type | Recommended Storage | Notes |
|---|---|---|
| Insulin | Refrigerate (2-8°C); Opened vials can be kept at room temp for 28 days | Freezing destroys insulin |
| Antibiotic Suspensions | Refrigerate (2-8°C) | Shaking required before dosing |
| Tablets & Capsules | Room temp (20-25°C) | Store in dry place out of sunlight |
| Biologics (e.g., Humira) | Refrigerate (2-8°C) | Don't freeze or shake |
| Eye Drops | Check label—some need refrigeration | Stability varies, do not freeze |
Mistakes happen. Maybe you left your medicine in a hot car or accidentally put a cream in the freezer. If you’re ever unsure whether your medicine is still safe, call your pharmacy. Don’t risk it—medication failures happen more often than you think because of storage mess-ups.

Common Myths and Misconceptions About Medicine Storage
Raise your hand if you’ve heard this: "Just put all medicine in the fridge; it’ll last longer." Sounds logical—sort of like sticking bread in the freezer, right? Well, it’s not always true. Some meds actually spoil faster if they’re refrigerated when they shouldn't be.
Here’s one for the books: Aspirin gets chewy and loses effectiveness if it absorbs moisture from a steamy fridge. Birth control pills stored in cold or damp conditions can lose their power—a risky game you don’t want to play. Oh, and storing medicine in the bathroom? Big mistake. Hot showers create humidity, and that ruins the integrity of most pills and tablets. Ever noticed those silica gel packs in vitamin bottles? They’re there to soak up stray moisture.
Even more surprising, there’s no "one-size-fits-all" rule for generics versus name-brand medicines when it comes to temperature. Both need to be kept under the same conditions—despite what someone on TikTok might claim. Some folks also believe expired meds are just "a little weaker." Actually, changes in temperature can make the chemical structure break down, making the drug not just less effective but sometimes harmful.
And let’s not forget the travel hacks people try. Sticking medicine in hotel minibars can backfire—many are much colder or warmer than you’d expect, and not reliable for sensitive drugs.
Tips for Storing Medicines Safely at Home
Finding the right spot at home to stash your meds doesn’t have to be tricky, once you know the ground rules. Start by reading—really reading—the label. Does it say "protect from light"? Then don’t leave it in a sun-filled spot. Is it telling you to refrigerate? Don’t just stick it next to the freezer coils; you want the main section, away from the back wall to avoid freezing.
Pick a spot away from heat, sunlight, and moisture. That rules out your bathroom and most kitchens. Most folks do best with a hall closet shelf, a bedroom drawer, or a temperature-stable pantry. To keep kids and pets safe, go high and consider using childproof containers or even a locked box for controlled medicines.
If your meds need refrigeration, make sure they’re not accidentally frozen. Store them in the fridge door or a middle shelf. If your power goes out, most medications can handle a few hours at room temp, but insulin and biologics may need to be tossed if they’ve been warm too long. In situations like camping or road tripping, invest in a travel cooler with a thermometer—some companies even make nifty portable medical fridges now.
When it comes to storing medicine, less is more—don’t keep old remnants or expired samples "just in case." And if the medicine changes color, develops a weird smell, or looks strange, it’s time for it to go.
When in Doubt: Ask the Right People and Use the Right Tools
Here’s the bottom line: when you’re not sure, turn to the experts—not social media hacks or hearsay. Pharmacists can double-check what’s safe for your specific prescription, and they can even give advice tailored to your hometown climate. If you want a techy edge, a simple fridge thermometer can ensure your fridge stays in that safe 2°C–8°C zone for your refrigerated meds.
If you travel a lot or live somewhere sweltering, there are medicine storage solutions made just for you—from insulated pouches to battery-powered coolers with built-in alarms if temps creep outside the safe zone. There’s even smart pill bottles that track temp and humidity, sending you alerts right to your phone.
And a golden rule: refrigerate medicine only if your label or pharmacist says so. Improvising can end up causing more harm than good. A few extra seconds of checking can mean the difference between your medicine saving the day—or letting you down when you need it most.